
Hormonal birth control is often seen as a convenient solution to many reproductive health concerns. From regulating periods to easing painful cramps, birth control is prescribed for reasons beyond pregnancy prevention. While its benefits are well known, the long-term risks are often overlooked.
One of the biggest concerns is that birth control can mask the symptoms of conditions like uterine fibroids, delaying diagnosis and treatment. Understanding both the benefits and the risks allows women to make more informed choices about their reproductive health and fertility.
Beyond Pregnancy Prevention: The Many Roles of Birth Control
Hormonal birth control prevents pregnancy by altering the levels of estrogen and progesterone, but its effects extend beyond contraception. Many women rely on birth control to manage heavy bleeding, cramping, and mood swings. Birth control is also used as a temporary solution to suppress conditions such as endometriosis and fibroids, which are fueled by fluctuations in estrogen.
Doctors often prescribe hormonal birth control for teens and young women to regulate menstrual cycles or manage painful periods. While this can provide temporary relief, some women continue using the same method for years without reevaluating whether it is still the best option.
What Health Risks Increase with Long-Term Birth Control Use?
While birth control is generally safe for many women, long-term use can carry risks that women should be aware of and discuss with their health provider.
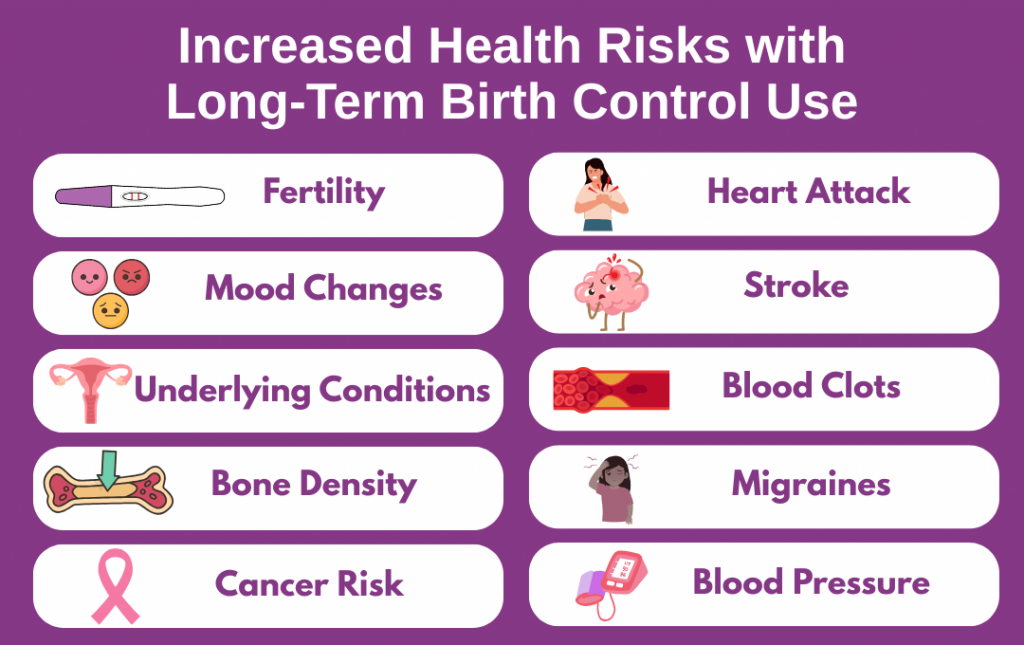
Fertility and Hidden Conditions
Research shows that hormonal birth control rarely causes permanent infertility. For most women, menstrual cycles return within weeks to months after stopping, allowing them to conceive.
However, birth control can mask the symptoms of underlying conditions such as polycystic ovary syndrome (PCOS), endometriosis, or fibroids. When these conditions go undiagnosed and untreated, they may progress over time, potentially making conception more challenging once birth control is discontinued.
Increased Risk of Heart Attack, Blood Clots, and Stroke
Certain birth control methods contain higher levels of estrogen, which are sometimes referred to as high-dose estrogen contraceptives. These include some combined oral contraceptives, patches, or vaginal rings.
High-dose estrogen can increase the risk of blood clots, which in turn may lead to stroke or heart attack. This risk is higher for women over 35 who smoke, as well as for those with additional health factors such as high blood pressure or a history of clotting disorders.
Cancer Risk
Studies show a slight increase in breast and cervical cancer risk with prolonged use of birth control, although it lends some protection exists against ovarian and endometrial cancers. Because cancer risk varies by individual and family history, regular screenings and open dialogue with a physician are essential.
Bone Density
Injectable contraceptives, such as Depo-Provera, contain the hormone progestin and are administered as a shot every 12 to 13 weeks to prevent pregnancy. While highly effective, long-term use has been associated with decreased bone density—a reduction in the calcium and minerals that give bones strength—which can increase the risk of fractures later in life. Bone loss is generally more concerning for adolescents, young adults, or anyone who already has low bone mass or other risk factors, such as a family history of osteoporosis, low body weight, smoking, or insufficient calcium and vitamin D intake.
For women using injectable contraceptives long-term, healthcare providers may recommend monitoring bone health with periodic assessments and taking preventive measures like weight-bearing exercise, adequate calcium and vitamin D, and lifestyle adjustments to protect bone strength.
Mood Changes, Blood Pressure, and Migraines
Hormonal birth control has been linked to a range of mental and physical health effects. Studies published in Lancet Psychiatry and Hypertension suggest higher risks of depression and elevated blood pressure among users, while the American Migraine Foundation warns that estrogen-containing contraceptives can trigger migraines and increase the risk of stroke.
While not every woman experiences these effects, they underline the importance of regular checkups and monitoring during long-term use.
How Birth Control Can Mask Underlying Reproductive Health Disorders
One of the most overlooked consequences of hormonal birth control is how it can effectively hide conditions such as fibroids, endometriosis, or polycystic ovarian syndrome (PCOS).
By suppressing menstrual cycles and easing pain, birth control may give the impression that the problem is resolved. However, birth control only manages symptoms while the underlying condition may continue to progress.
When birth control is discontinued—often when a woman is trying to conceive—underlying gynecological conditions, such as fibroids, endometriosis, or PCOS, can resurface, sometimes more intensely than before. This highlights the importance of regular check-ins and early evaluation to ensure that any reproductive health issues are identified and managed properly.
The Connection Between Birth Control and Fibroids
Uterine fibroids are noncancerous tumors composed of muscle and fibrous tissue that develop in the uterus. They are among the most common gynecological conditions, affecting an estimated 26 million women aged 15 to 50 in the United States.
Hormonal birth control is often used to manage fibroid-related symptoms such as heavy bleeding or painful periods. While it can provide temporary relief, it does not shrink or remove fibroids.
Recognizing the Symptoms
Common symptoms of uterine fibroids include:
- Heavy or prolonged menstrual bleeding, often with large blood clots.
- Pelvic pain or pressure, which may be constant or intermittent.
- Frequent urination or difficulty emptying the bladder.
- Constipation or bloating.
- Pain during intercourse.
- Lower back pain.
- Enlarged abdomen, giving a sensation of fullness or bloating.
- Fatigue or light-headedness, often due to anemia from heavy bleeding.
If you’re experiencing any of these symptoms, it’s important to pay attention to your body and take note of changes over time. Use our symptom checker to help identify potential warning signs and guide your conversation with a healthcare provider.
Importance of Early Detection of Fibroids
Because birth control can mask fibroid symptoms, many women dismiss what their bodies are signaling. This often delays diagnosis until symptoms become severe or interfere with fertility. By then, fibroids may be larger and harder to treat.
Paying attention to changes in your cycle, asking questions, and seeking medical evaluation early can open the door to more treatment options. Some treatments can manage fibroids or other gynecological conditions while still allowing you to have children, while others, like a hysterectomy, remove the uterus and make pregnancy impossible. Getting care early gives you more choices to protect your reproductive goals.
How Fibroid Fighters Supports Awareness and Early Action
Fibroid Fighters is dedicated to raising awareness about fibroids and the importance of early diagnosis. By sharing real stories and building community, we help women understand their symptoms and make informed decisions about their care.
If you are managing symptoms with birth control or have concerns about fibroids, Fibroid Fighters provides educational resources and personal stories from women who have navigated similar experiences. Follow us on social media to read these stories, learn more about fibroids, and join a community that empowers women to take charge of their reproductive health.







