
Did you know that diabetes or prediabetes may increase your risk of developing uterine fibroids? Diabetes affects over 38 million Americans, and it’s crucial to be aware of its potential complications, especially for women’s health.
While the exact cause isn’t always clear, research suggests a connection between insulin resistance, a common complication of diabetes, and the development of these fibroids.
What is Diabetes?
There are two main types of diabetes. Type 1 diabetes is an autoimmune disease where the body attacks its own insulin-producing cells. Type 2 diabetes is a condition where the body becomes resistant to the insulin it produces or doesn’t make enough of it.
Insulin is a hormone secreted by your pancreas that allows your body to metabolize glucose (sugar) into energy. When your body doesn’t use insulin effectively, the result is high blood sugar, or hyperglycemia.
Sustained hyperglycemia can lead to health issues such as degraded sight, kidney failure, and venous insufficiency. People with diabetes are also more at risk for skin ulcers and amputation of the limbs.
The Higher Risk: Diabetic Statistics
Risk factors for diabetes include family history, age, weight, and physical inactivity. Importantly, risk is disproportionately higher among certain ethnic groups:
| Ethnicity (Adults) | Prevalence of Diagnosed Diabetes |
| Non-Hispanic Asian Americans | 9.5% |
| Non-Hispanic White Adults | 7.4% |
| Hispanic Adults | 11.8% |
| Non-Hispanic Black Adults | 12.1% |
| American Indians/Alaska Natives | 14.5% |
The American Diabetes Association recommends starting routine screening every three years from the age of 45. However, if you have additional risk factors, it’s advised to consult your healthcare provider for more frequent screenings.
The Hormonal Bridge: Diabetes, Insulin, and Fibroids
Uterine fibroids are non-cancerous growths that are made up of smooth muscle cells and fibroid connective tissue. The hormone estrogen primarily fuels these growths.
The connection between diabetes and fibroids is rooted in hormones and growth factors:
- Insulin Resistance Hyperinsulinemia: When cells resist insulin, the pancreas produces more insulin to compensate. This excess insulin, called hyperinsulinemia, is a powerful growth signal.
- Growth Factor Stimulation: High insulin levels stimulate the production of Insulin-like Growth Factor-I (IGF-I). Both hyperinsulinemia and IGF-I are known to act as growth promoters for fibroid cells.
- Increased Free Estrogen: Hyperinsulinemia also suppresses the production of Sex Hormone-Binding Globulin (SHBG). Lower levels of SHBG mean more free, active estrogen is circulating in the blood, which directly feeds fibroid growth.
Key takeaway: uncontrolled diabetes and insulin resistance create a pro-growth environment for estrogen-dependent tumors like fibroids.
Do Fibroids Affect Blood Sugar Levels?
While the relationship between diabetes and fibroids is well-documented (with insulin resistance fueling fibroid growth), current research suggests that uterine fibroids do not directly cause or significantly raise a woman’s blood sugar levels (hyperglycemia).
Fibroids are growths primarily fueled by estrogen and various growth factors (like IGF-I). They function as estrogen-dependent tumors within the uterus, but they are not known to produce hormones that directly regulate or interfere with insulin production or glucose metabolism in the bloodstream.
However, fibroids can impact a woman’s overall metabolic health in ways that are relevant to blood sugar management:
- Anemia and Fatigue: Large or multiple fibroids often cause heavy and prolonged menstrual bleeding, which can lead to severe anemia and chronic fatigue. This persistent exhaustion can make it significantly harder for a woman to maintain the lifestyle habits essential for managing blood sugar, such as regular exercise and consistent healthy eating.
- Hormonal Feedback Loop: Though fibroids don’t directly raise blood sugar, the increased estrogen levels associated with fibroid growth can be linked to conditions that do impact blood sugar, such as polycystic ovary syndrome (PCOS). Both PCOS and fibroids are associated with insulin resistance, creating a complex hormonal and metabolic environment where the two conditions can co-exist and worsen one another.
In summary, fibroids themselves are not an endocrine factor that drives up blood sugar, but the secondary effects of fibroids—like severe fatigue and anemia—can complicate and undermine a woman’s efforts to control existing diabetes or prediabetes. Addressing the fibroids can therefore be a critical step in achieving better overall metabolic control. .
Recognizing Fibroid Symptoms
It’s important to know the symptoms that indicate you might have fibroids, as many women are unaware that these signs may mean something is wrong.
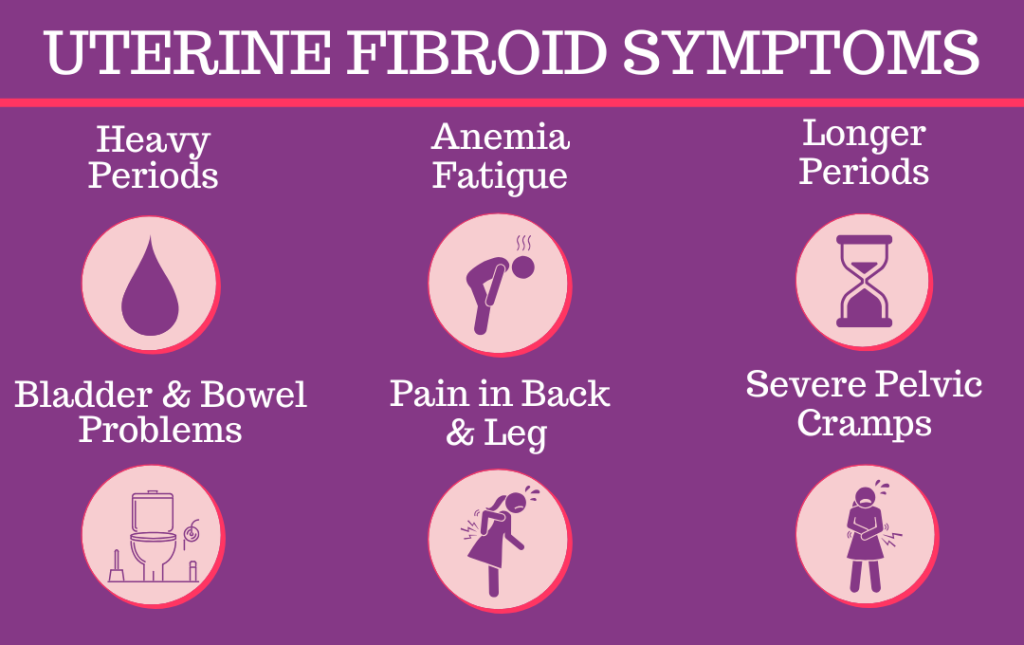
Signs of fibroids include heavy and/or more extended periods; anemia; bladder or bowel problems; back or leg pain; and severe pelvic cramps.
Is There a Connection Between Diabetes and Fibroids?
A recent study explored the relationship between insulin-like growth factor II (IGF-I) and its role in the development of fibroids. The study found that both conditions share some of the same risk factors, such as obesity, family history, and age.
Diabetes may conceal the presence of fibroids because it alters hormone levels and raises blood sugar levels which can cause lengthy, heavy, irregular menstrual cycles and exhaustion.
If you are living with or are at risk for diabetes, it is vital to pay attention to your body and note when something is amiss. Inform your doctor if you experience new or troubling symptoms.
Impact on Reproduction and Period Health
Poorly controlled blood sugar levels can disrupt the delicate hormonal balance necessary for ovulation, leading to irregular or absent menstrual cycles. In pregnancy, high blood sugar significantly increases both the mother’s risk (e.g., pre-eclampsia) and the baby’s risk (e.g., macrosomia and birth defects).
However, recent advances in insulin therapy, including new formulations and precise pump delivery, have significantly improved menstrual management for women with diabetes, making it easier to adjust insulin levels based on hormonal fluctuations.
Steps You Can Take for Better Health
The best way to advocate for your health is to focus on a shared solution: improving insulin sensitivity.
Track Symptoms: Pay close attention to your body. If you are living with diabetes and notice a severe change in your menstrual cycle—like heavy bleeding that leads to anemia or debilitating pelvic pressure—do not dismiss it. Inform your doctor and request a fibroid screening.
Lifestyle Fixes: Weight management and regular exercise are the most powerful tools. Losing even a small percentage of body weight (5-7%) can drastically improve insulin sensitivity and potentially slow the growth factors that feed fibroids.
Take our one-minute symptom checker to learn if you are suffering from fibroids here.
What To Do If You Suspect You Have Uterine Fibroids
Inform your doctor if you experience irregular periods, a sudden urge to urinate, or fatigue.
Fibroid specialists can accurately diagnose your illness and pinpoint fibroid tumors using image-guided technologies such as ultrasound and magnetic resonance imaging (MRI).
If you’re diagnosed with fibroids and worried about surgery and its impact on your fertility, there’s a less invasive, outpatient procedure that offers a quicker recovery and minimal disruption to your daily life. Uterine fibroid embolization (UFE) treats all uterine fibroids simultaneously and relieves uncomfortable symptoms.
At the Fibroid Fighters Foundation, we aim to educate women with fibroids about their treatment options. If you’re experiencing symptoms and want to get checked for fibroids, give us a call at 855-455-5262 or contact us online.
The Fibroid Fighters Foundation is passionate about connecting women with one another to share their unique stories about living with fibroids. If you want to share your fibroid journey and connect with others, check out our testimonial page here where you can talk about your experience via video, audio, or text.
References:
- https://journals.sagepub.com/doi/full/10.1177/2042018819895159
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2856640/







